Hello everyone! I’m Chloe, the new Practice Manager at Driving Well. With three months under my belt, I’m excited to share my journey into the world of allied health business, occupational therapy, driving, and the NDIS.

The Journey to Driving Well
My background in biomedical science and my mother’s influence as a nurse sparked my interest in healthcare. However, my role as a sleep scientist left me feeling unsatisfied. The listing for a Practice Manager at Driving Well caught my eye, offering a way to help people achieve their goals of driving. The fantastic team culture and opportunities have made my transition rewarding and fulfilling.
A Day in the Life of a Practice Manager
My role as Practice Manager keeps me on my toes, with each day bringing new clients, questions, and projects. I’m the one to greet you on the phone and help you book your appointments to get back on the road. However, there is much more to my role than just scheduling. I handle finances, send reports, and work on various projects and developments within the business. There’s no such thing as a typical day or week here!

Top Three Learnings
My first three months have been a whirlwind, filled with valuable lessons:
Patience:
Navigating the NDIS can be tricky, slow, and sometimes frustrating. I’ve learned the importance of patience, understanding that good things take time. Working through the many processes and hoops required to help clients get back to driving or start their journey has been a significant learning curve.
Diversity:
With over 130 clients in just a few months, I’ve witnessed incredible diversity in conditions, cases, and goals. This experience has highlighted that there’s no “one size fits all” in occupational therapy. The endless possibilities in helping people have been a heartwarming revelation.
Organisation:
Organisation is key in my role. Ensuring all paperwork is in order before assessment day can be stressful, but I’ve developed effective methods to ensure smooth sailing for everyone involved. My advice: have your paperwork ready on time to avoid unnecessary stress.
Exciting Projects Ahead
I’m working on several exciting projects at Driving Well:
Enhancing the toolkit with new content and making it more accessible for clients who can’t visit the clinic.
Physical Get Driving Toolkit:
Developing a tangible toolkit to send to clients, complementing the digital version.
Theratrak:
An online tool to aid clients in their therapy exercises from home. This tool allows assigning exercises and maintaining contact with clients between appointments to develop their pre-driving skills further.
Practice Manager’s Academy (PMA):
A personal project where I am developing my skills as a practice manager, thanks to the opportunity provided by Jenny.
Top Tips for Booking a Driving Assessment
Here are my top three tips for clients preparing for a driving assessment:
Breathe:
It’s normal to be nervous. The Driving Well team is supportive and ready to answer all your questions. Remember to take deep breaths and stay calm.
Be Patient and Kind:
Organising driving assessments involves coordinating with multiple people. While the team works efficiently, sometimes things don’t go as planned. Patience and kindness go a long way in making the process smoother.
Read What We Send You:
Ensure you read all the information we send you. This will cover everything you need to know about your appointment, from the location to what to expect before, during, and after the assessment. Being well-informed will save you from potential headaches.
I’m excited to thrive in my role and look forward to the positive impact I’ll continue to make at Driving Well!
Brisbane OT driver assessors were recently provided the opportunity to practice driving with vehicle mods with Total Ability and our specialised driving instructors, at the RACQ Mobility Centre at Mount Cotton.

Driving OTs frequently work with clients with physical injuries, conditions and disabilities which may impact their ability to use conventional vehicle controls independently and may need modifications to enable them to drive. There are a multitude of driving modifications available, including various types of spinner knobs, hand controls, left foot accelerator pedals, through to higher level / advanced modifications such as the mini wheel and joystick steering, and driving from wheelchair.
Driving OTs are skilled at assessing clients’ functional abilities and work together with the client and a suitable driving instructor, to work out what driving modification will best suit the client and their situation. The driving OT will also guide the client on the process that is required for them and support them with applying for funding for driving lessons and funding of the modifications, guide them through the licensing process, and explaining the engineering and compliance process.
What we are not necessarily skilled at, is actually driving with the modifications themselves!
Having a professional development day offline, in the company of our friends and colleagues, in a safe and supported environment to practice driving with the various vehicle mods on a closed track (no traffic!) was just invaluable.
Myself, Zoe and Amanda were all able to attend and between us, we practiced driving with:
- Fadiel e-radial hand control and spinner knob
- Fadiel trigger hand control and Lodgesons lollipop spinner knob
- Basic push-pat mechanical hand control and spinner knob
- Left satellite accelerator and right brake lever
- Left satellite accelerator and left Fadiel easy drive brake (I didn’t think this would be do-able, but after a client demonstrated this with ease, I was up to the challenge and yes it certainly can be done!)
- Left mini-wheel advanced electronic steering and right two-way joystick (brake/accelerator) drive from wheelchair
- Left foot accelerator (for me, this is still the hardest way to drive – I am not coordinated with my feet at all)
- Four-way joystick (brake, accelerator and steering all-in-one) drive from wheelchair – I was not game to test this one out… kudos to the driving OTs that did.
Biggest takeaways for our team were:
- it was useful to remember the functional components required to drive with each of the modification types
- “unlearning” of our standard recommendation – the technology and techniques have advanced and grown, so our previous go-to (which still works) might not be the only option.
- There are so many options, that it is really up to what suits the client best, and that they may need several trials to settle on the right modification for them.

Sharing a huge congratulations again to Paul Crake and his team at Total Ability once again for their efforts which were rewarded at the May ATSA conference in Brisbane, with Paul taking out not one, but three awards for:
- Commitment to Excellence (shout out too to Ali Akbarian at Mobility Engineering – sponsor of the Drive-Able podcast
- 2024 Industry Person of the Year
- 2024 Supplier / Manufacturer of the year
Total Ability have dedicated time and resources to supporting the driving and disability industry and have developed several resources to assist clients and OTs understand the vehicle mods process.
For anyone needing vehicle modifications to return to driving, there will be an involved process that will likely include:
- OT driving assessment (including a clinical and practical on-road assessment; multiple trials may be necessary to find the best option)
- OT driving assessment report and recommendations for funding
- Driving lessons with the driving instructor to develop competency and safety – “is this consistent and reliable?”
- Applying for vehicle modifications funding (eg to the NDIS, NIISQ, i-Care, TAC, HCP)
- Completing an on-road re-assessment / handover assessment upon completion of the modifications, and a post-modification report.
Helping drivers return to driving or learn to drive with vehicle mods is one of our favourite things to do – that handover day to see a client driving away with their vehicle and regaining their independence, is absolutely magical to us.
If you need assistance with returning to driving, please check out our website or make a referral!
People with Motor Neurone Disease go through huge changes in their daily life, incredibly quickly. All of a sudden they are unable to stand up by themselves, walk to the bathroom, go out to the shops as they previously did. All of a sudden they are unable to do the things we take for granted every day.
One man I worked with recently had this same story.
The problem…
All of a sudden he was having black outs and couldn’t walk any more. He was quickly provided with a hire wheelchair to get him by until he could get a scripted power wheelchair more suitable to his needs. When I met him in September he was still transferring into a standard car, but I knew this could change really fast. It is so important to think about the future – for MND, things can keep changing really quickly and we need to plan for the worst case scenario, and any vehicle mods solution that we recommend needs to be safe, consistent and reliable, and sustainable. It also needs to meet the insurers “reasonable and necessary” requirements.
I explained the options to to this fellow and his family, and showed a few options on vehicle modifier websites.
The lowered floor conversion to a Kia Carnival is a really effective, popular, and affordable solution, and many Australians use this option. The other options that are also equally effective include the Hyundai Staria and Volkswagen Multivan.
The trial…
The Kia Carnival looked like the way to go in this case, so I quickly commenced the process of trialling and applying to NDIS for vehicle modifications to his Kia Carnival to enable him to transport in his power wheelchair.
The trial was at the client’s home, and allowed him the opportunity to drive up into the car in his electric crashtested wheelchair, see how the restraints work, and go for a test drive. It was all smooth sailing. I gathered all the paperwork needed (there is a lot), and submitted an application to the NDIS to have the modifications funded. The client is responsible for purchasing the actual car.
The approval…
By the end of February 2024, we received approval from NDIS to proceed with vehicle modifications. This is a pretty quick turn-around time in the NDIS world. But, within this time he had lost his ability to transfer into a standard car seat. By the time the approval came through, he’d been stuck at home for 2-3 months, unable to go anywhere over the Christmas period. His hire wheelchair was not suitable for transport, and he couldn’t transfer out of it. Imagine that – being stuck in your own home over Christmas, not being able to take your kids out to celebrate the school holidays, not able to go Christmas shopping, not being able to visit family.
So, the NDIS approval came through at the end of February. Blair and his team at KM Kite on the Gold Coast bent over backwards to schedule the modifications and make it happen as quickly as possible. A job that usually takes 6-8 weeks minimum, they got sorted in less than 4 weeks. They also managed to get him a hire car NDIS had approved funding for so he could transport in the meantime. By the end of March, he had his Kia Carnival with passenger modifications for wheelchair occupant travel.

The solution!
Have a look at the smile on his face!
Lowered floor Kia Carnival delivered with a big blue bow!
He was stoked he could finally, again: be a part of taking his kids to school, going to the shops, going out to watch the footy. All the activities we take for granted every day.
His story really highlights the need for supports to be quickly accessible for people with MND, and the need for increased awareness around the challenges they face.
Zoe Wagner-Jordan, OT Driver Assessor, Driving Well Occupational Therapy
Need to get out and about?
please get in touch or have a look at our website for more information!
Learning to drive is an exciting rite of passage for young people. It can be the beginning of their life as a young adult, independence, trips with their friends – no more pick up and drops off for parents!
As exciting as it may be for the young person, it’s often a daunting prospect for parents.
- Are they ready?
- Will they be safe?
- How will I survive giving them lessons?
- What if they don’t pass?
Learning to drive requires a massive energy, time and monetary commitment. It takes time and practice to learn road law theory, courage to sit the exam (once or twice!) and even more courage to sit in the passenger seat as your child takes the wheel. Add to the mix, a learning disability, autism, ADHD, anxiety or physical impairment and it can seem an unclimbable mountain.
At Driving Well, we’re here to help you through this process.
Our Potential to Drive Program provides a starting point for learner drivers with additional needs who may be thinking of getting their learner’s permit or starting driving lessons. We provide comprehensive assessment to uncover the learner’s/your child’s learning needs based on their disability and work closely with specialised driving instructors to put together a learning package just for them.
We can also provide you with advice on what you can do in day-to-day life to build the skills they need to be a successful driver and support linking with formal therapies that may help. We also offer support for parents and caregivers to learn how to practice skills on-road skills with the individual and to learn the techniques used by their driving instructors to minimise lesson stress!
We can support you through the process of seeing if learning to drive can be supported by your NDIS Plan and walk you through the process form start to finish.
This is a huge undertaking and not a simple process. It is really important that we have a partnership between Driving Well OT and the client and their family.
Read more about the OT “potential to drive” process here.
Approval for driving training program
When a driving program (lessons) are recommended, the OT driver assessor will submit the OT driving assessment report and quote for the number of recommended lessons from the driving instructor provider, to the NDIA
“specialised driving training” is a quote required item, which needs to be approved by NDIA and added as a line item to your NDIA plan under Capacity Building: improved daily living (Specialised driver training 15_046_0129_1_3) this applies even if you have a goal regarding driving / community access, and even if you have sufficient budget in improved daily living.
Once you have written approval from the NDIA (and the line item is added to your NDIS plan), you are able to book your lessons directly with the driving instructor. (Note – as at February 2022, this is taking months to gain approval).
If you are with another insurer, a quote and report is provided, and the insurer must approve the quote to commence lessons.
Drive Focus App
Drive Focus is a tablet based app (ipad/android tablet) designed to develop visual search, reaction time/processing/decision and motor execution skills (the information processing model) required for driving.
- It has interactive video taken from the driver’s perspective, which is coded with tap-able “hotspots” of the critical items: brake lights, stop signs, traffic lights, speed signs, pedestrians, cars entering from left/right, objects on the road). The user must tap on the critical items as quickly as possible in the correct order.
- The app has Australian “tours” of Brisbane and Melbourne available and costs approximately $20AUD; there are seven drives within each tour, each of increasing difficulty.
- Visual cues for critical items can be turned on and off, and the videos can be slowed down to allow more processing time.
- The user’s score is presented at the end of each practice, and android users can email their results to their OT.
- A university study identified that six one-hour sessions of Drive Focus significantly reduce driving errors among already licenced drivers. The subjects also rated Drive Focus as valuable for improving their driving skills.
- There are other studies taking place in the USA and Canada presently to examine the efficacy of Drive Focus with populations including older adults post stroke, traumatic brain injury, and combat veterans with post-traumatic stress.
Our learner drivers are recommended to practice the app three to four times per week for about 15 minutes each session; they can level up through the drives, and review their score and re-attempt to improve their score (number of critical items and average response time).
The app is a Finalist for Best Assistive Technology product at the upcoming Australian Disability Service Awards, and winner of the Technology Award for Australian Road Safety Foundation 2021!
Why should I purchase the Get Driving toolkit?
Driving lessons are full-on – there is a lot to take in, especially in the early phases.
We know for conditions including ASD and ADHD that focusing on one task at a time and building this up (eg developing visual searching skills when outside of the car or when in the front passenger seat) will then make it easier to integrate skills when behind-the-wheel on driving lessons.
Driving Well has developed a therapy program (face to face clinic and passenger activities) and this online therapy toolkit for clients to purchase access at home with their parents / support workers, to work on fundamental skills needed for driving – and build these up so they will get more out of their driving lessons with the driving instructor.
Therapy program sessions at our new clinic space!
We are renting a clinic space at Takes Care Specialist Centre, 11 Cleveland St, Stones Corner on Wednesdays, commencing 16th November. We are so excited to be able to provide “Get Driving” therapy programs to our learner driver clients at this beautiful and accessible clinic space. This will reduce costs to our clients, and allow us to be so much more efficient in providing services.
Need support with driving and vehicle modifications assessments? Email admin@drivingwell.com.au to see if we can help you.
Article by Lauren Jackson OT Driver Assessor and Jenny Gribbin OT Driver Assessor

Blog by Zeta Griffiths, Practice Manager extraordinaire
Photo : Zeta and Jenny (Director of Driving Well)
From an intake perspective the best advice I could give to any client would be, be involved in the process.
Our OT team is amazing, but they aren’t mind readers. A lot of the important information will come from you. For example…. What are your capabilities and limitations? Do you really have 20/20 vision, or might the Optometrist have a different opinion of your eyesight. The information that you gather for us before you actually meet your OT for the first time is invaluable.
Be prepared, make that appointment with your GP (make sure it’s a long one) and don’t leave without the paperwork we’ve asked you to get. Sometimes the GP thinks they know the process and can be a little stubborn, be patient and insistent and it will save you a second trip back to see them if you don’t come away with what we need.
Sometimes there are other things holding people back from getting everything organised. You may need a family member to take you for the appointments or you have scanner or fax limitations. Don’t get too hung up on how I’m going to get the paperwork back, I’ve got a whole bag of tricks up my sleeve. Get the process started and we’ll help you with the returns policy 🙂
I was once told I was being a pest by a lovely young man (98 years young) who needed an assessment. He didn’t have his paperwork and his assessment was quickly approaching. I would call him every second day, and ask if he’s made his appointments with the GP and Optometrist. He knew he needed to get them, but something was holding him back. On my last call to him I asked him what was really stopping him? His answer, “it’s time to stop and I just didn’t want to admit it. Not to mention Zeta, I though about what you said about all the money I’ll save when I get rid of the car and insurances etc and you know what, that’s a lot of beer!” We had a laugh and he gracefully retired from driving.
Everyone’s situation is different and our team would like to help you find your destination.
Our website explains in detail the process and forms needed for an OT driving assessment:
Email your referral to admin@drivingwell.com.au for support with driving assessments and vehicle modifications.
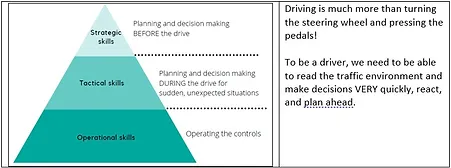
For experienced drivers, it is easy to forget just how complex driving is….. what do you think driving involves? Steering the steering wheel? Using the pedals? Indicating? Keep going, you’ll think about scanning, procedures, taking safe gaps, following the road rules… however, driving is much more than turning the steering wheel and pressing the pedals! To be a driver, we need to be able to read the traffic environment and make decisions VERY quickly, react, and plan ahead.
Michon’s model of driving performance outlines three areas of skill required for driving:
- Operational skills: basic operation and decision in routine situations – eg operating the pedals and steering wheel for basic control of the vehicle – managing intersections, speed control, observing traffic environment.
- Tactical skills: complex decision making in non-routine situations – eg more complex intersections and decision making (eg busy multilane roundabouts/cross intersections), highspeed situations, managing complex carparks, roadworks zones, detours, traffic jams, adverse weather conditions, self-navigating in unfamiliar areas, wrong turns.
- Strategic skills: being able to plan driving ahead of time – eg need to be at work at 11, therefore have to start getting ready by 10 and leave by 10:30am; need to get fuel, need to check tyres/air pressure, need to check for flooded roads.
Michon’s model:
The Assessing Fitness to Drive Guidelines 2016 (the ‘bible’ used by medical and health professionals for driving and medical conditions) states:
Driving is a complex instrumental activity of daily living. It involves a complex and rapidly repeating cycle that requires a level of skill and the ability to interact with both the vehicle and the external environment at the same time. The demands of the driving task can vary considerably depending on a range of factors including those relating to the driver, the vehicle, the purpose of the driving task and the road environment. Information about the road environment is obtained via the visual and auditory senses. The information is operated on by many cognitive processes including short- and long-term memory and judgement, which leads to decisions being made about driving.
Decisions are put into effect via the musculoskeletal system, which acts on the steering, gears and brakes to alter the vehicle in relation to the road. This repeating sequence depends on:
- Sensory input: vision, visuospatial perception, hearing
- Cognitive function: attention and concentration, comprehension, memory, insight, judgement, decision making, reaction time, sensation
- Motor function: muscle power, coordination.
Given these requirements, it follows that many body systems need to be functional in order to ensure safe and timely execution of the skills required for driving. The driver’s sensory, motor and cognitive skills may require detailed assessment to determine the potential impact on driving.
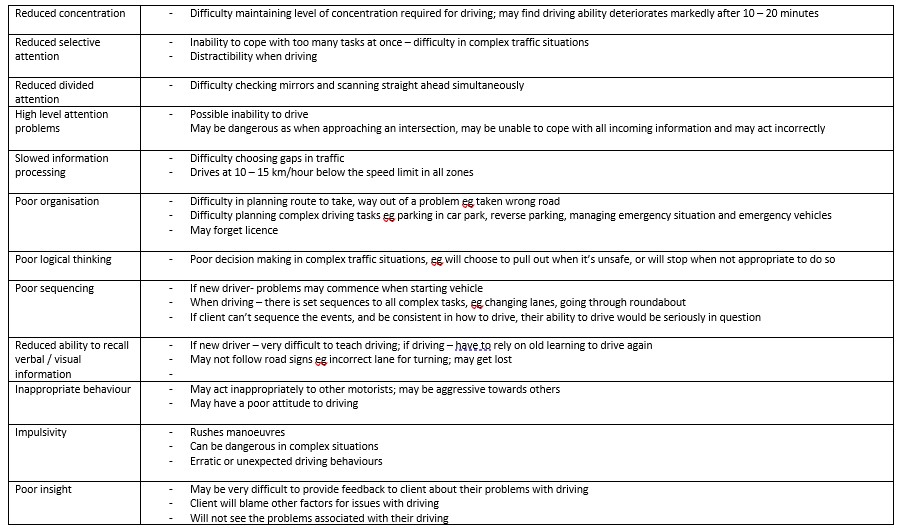
In simple terms, cognition is our memory and thinking skills – it allows us to read and make sense of the environment, to make decisions, to react in a timey manner, to have awareness of errors and correct these, to learn. Without sufficient cognitive functioning, driving is impossible.
Occupational therapy driver assessors include a thorough screen of cognitive functioning in the clinical or “off-road” part of the driving assessment, and then this is reviewed practically during the on-road driving assessment.
Clients may have impairment of cognition due to various reasons – eg stroke, brain injury, other neurological conditions such as Parkinson’s disease and Huntington’s disease, Alzheimer’s/Dementia, or a mild cognitive impairment which may be associated with age-related changes. For many people, getting older can lead things generally slowing down – including slowed speed of information processing – that is, taking longer than it used to, to read the situation, react and make decisions. This often doesn’t impact on day-to-day tasks – it doesn’t really matter if it takes a little longer to do the grocery shopping, cook a meal or do a puzzle – but it is a HUGE problem when it comes to driving. To be a safe driver, we need to be consistent and reliable with being able constantly observe the traffic environment (and not miss any signs or hazards), react and make decisions accordingly.
The table below outlines different aspects of cognition, and how these may impact on driving.
What does this mean for driving?
There are three possible outcomes from any occupational therapy driving assessment:
(Definition: A critical error is where the driving instructor has to intervene on the steering wheel / brake / accelerator for safety – this is only done when absolutely needed, and the client is given a chance to recognise and react themselves, prior to the instructor intervening).
“Pass”: medical condition is not impacting on driving and therefore safe to continue driving.
In practice, this would mean:
- in the clinical / off-road assessment: there would be appropriate performance
- in the practical assessment: no critical driving errors, minimal non-critical driving errors, aware of errors, acknowledging feedback from driving instructor and OT, implementing feedback consistently.
“Driving program: trial of lessons”: client has not yet passed – requires lessons / refresher sessions with the specialised Driving Instructor to attempt to address concerns seen in the initial on-road assessment or learn to drive with vehicle modifications. In practice this would mean:
- in the clinical / off-road assessment: some concerns in the cognitive tests
- in the practical assessment: critical and non-critical driving errors, showing some awareness of errors, making an attempt to implement feedback, but inconsistent with this.
- recalling the feedback and errors after the assessment
- being open to learning and improving their driving
“Fail”: medical condition is impacting on driving and no longer safe, and recommendation that the licence will be cancelled and the person is recommended to retire from driving.
- In practice, this would mean:
- in the clinical / off-road assessment: poor performance in the cognitive tests
- in the practical assessment: critical and non-critical driving errors, not aware of errors or driving instructor intervention, not able to implement any feedback or make any improvements with driving
- not recalling feedback or errors after the assessment
- poor memory to be able to remember strategies to improve driving
- poor awareness/insight into medical condition and driving performance
Safety first....
Safety trumps everything…. most people can operate the car (steering and pedals), but if they are not reading the environment appropriately and not processing things quickly enough – this is not going to be safe, and this means that it is time to retire from driving.
#occupationaltherapydrivingassessment #cognition #olderdrivers #neurologicalconditions #retiringfromdriving
References:
Michon, J. A. (1985). A critical view of driver behavior models: What do we know, what should we do. In L. Evans & R. C. Schwing (Eds.), Human behavior and traffic safety (pp. 485–520). New York: Plenum Press.
When a person can’t use their lower limbs for operating brake/accelerator anymore (eg due to an injury such as lower limb amputation, or medical condition such as diabetes or multiple sclerosis), they will often be able to return to driving by using hand controls – this is where they have a lever that comes out from the steering column for braking, and then various different options for accelerating.
Two main types of hand controls: mechanical and electronic:
Mechanical hand controls
How do they work: “push-pat” – push the brake lever forwards for braking (braking is ALWAYS push forwards – because as humans we tend to put our hands out in front of us to stop us from falling), and “pat” it down for accelerating. This style has two rods that run down through the steering column, that connect to the pedals, so when you push the hand control, they activate the pedals.
For steering, a spinner knob is required to be able to operate the steering wheel safely with one hand. This is a requirement of all State Licencing Authorities, and a requirement of the governing guidelines AS/NZS 3954:2019 Motor Vehicle Driver Controls: adaptive systems for people with disabilities.
From left to right below:
Young fellow had his precious (and old) Ford Falcon, so had push-pat hand controls installed; close-up of push-pat hand control with electronic indicator panel, and close up of push-pat hand control with green toggle switch indicator.
Suitable for: these are a basic hand control that work well for older vehicles.
Problem: cars with knee airbags
- For newer vehicles, if they have a knee airbag (an airbag positioned near your right knee under the dash board, the mechanical hand controls ARE NOT compatible – if the knee airbag is deployed in a collision, then the airbag will snap the rods into your legs – definitely not good.
- Technically the knee airbag can be deactivated, but Transport authorities don’t like this (you need to apply for an exemption), and it may void the manufacturers warranty. The solution for newer vehicles that do have a knee airbag is electronic hand controls.
- This is old tech… it is on its way out… if these are installed, then the client upgrades their car which has a knee airbag, they will need to re-learn the new electronic hand controls and go through the whole driving assessment process again.
Electronic hand controls
How do they work: the brake lever is still connected to the pedals, so push forward on the lever activates the brake. This is typically positioned on the right hand side but can be trialled in some driving instructor vehicles on the left side. We usually like the stronger hand to operate the brake – stopping the car is the most important function in driving!
Then there are multiple options for accelerating – it depends on the person’s abilities such as dexterity, strength, sensory issues, any pain/fatigue. Common types are:
- Trigger accelerator: suitable with good finger dexterity – the index finger squeezes a small “trigger” to accelerate. A spinner knob is required on the steering wheel to steer safely with one hand. Indicators can be used on the hand control or on the spinner knob.
- E-radial or T-radial accelerator: suitable when there is poor finger dexterity – the hand/wrist/forearm rotates slightly to accelerate. A spinner knob is required on the steering wheel to steer safely with one hand. Indicators can be used on the hand control or on the spinner knob.\
- Satellite accelerator: this is a corded or wireless option device that sits on the back of the left hand, and thumb is used to squeeze a small lever to accelerate; also use the brake lever and standard indicators. Tricky to master, but a great option when two hands need to stay on the steering wheel due to shoulder strength issues. In my experience, this usually suits people with a car racing background.
- Overring accelerator: the accelerator is a ring that is installed onto the top of the steering wheel, that you squeeze gentle inwards to accelerator; still use the brake lever, steering wheel for steering and conventional indicator. Again, tricky to master but a great option where there is reduced shoulder strength; this is only available in one vehicle in Brisbane for trial.
- Carospeed hand control system: this is operated with the left hand, the hand control is pushed forwards for braking and pulled backwards for accelerating, indicators can be wired in, and a spinner knob on the right hand side. This is only available in one vehicle in Brisbane for trial.
From left to right below:
Female driver using the trigger accelerator; male driver using the satellite accelerator; female driver using the overring accelerator; close-up of the Fadiel FSK2005 brake lever/trigger accelerator; close-up of the Fadiel e-radial accelerator; close-up of the satellite accelerator; close up of the Carospeed hand control system (left side operated); male driver using the trigger accelerator.
Higher level needs
For people with higher level disabilities (eg quadriplegia) who need a little extra help, then the next level of hand controls are full electronic input systems – such as the mini-wheel or joystick, and “Freedom” brake/accelerator units. These are available from Problem Management Engineering and Total Ability and require very intensive assessment and trials, and intensive training.
Process
Getting back on the road with hand controls is a bit of a process, but so worthwhile. These steps will guide you through the process (bearing in mind the licencing process may vary from state to state – this is the QLD flavour)
1. Referral / intake
- Get a referral and QLD Transport Medical Certificate from your GP
- QTMC must state: “medically stable for purpose of OT driving assessment / lessons with driving instructor only”, and tick “M” medical condition and “V” vehicle modifications boxes
- take the completed QTMC to the QLD Transport office for processing – you will get an updated licence with these conditions according to the QTMC; you MUST check the expiry date and gain an updated QTMC when this expires!
2) OT driving assessment: clinical and practical assessment, to trial various hand controls.
At intake, your OT driver assessor should be able to work out with you which type of hand controls you will be most suited to, and book a specialised driving instructor with these type of controls in their vehicle.
If we haven’t nailed the hand control choice, we will do further drives in the same vehicle/hand controls to get a bit more practice and confirm, or we may do further drives with different hand controls (same instructor/vehicle or different instructor/vehicle).
If we’ve worked out the right hand controls for you, we’ll discuss the recommended number of lessons – this will vary between 5 to 10 lessons, right through to 15 to 20, or even 30 to 40 for high level electronic gear, dependent on previous driver experience (some clients are teens / learners and have never driven before) and your progress.
3) Recommendations and paperwork
Once a decision on the hand controls is made, the OT driver assessor completes report/s and obtains quote for driving lessons from the chosen driving instructor, which is submitted to the insurer for approval.
NDIS information:
When lessons are recommended, the OTDA will submit the OT driving assessment report and quote for the number of recommended lessons from the driving instructor provider, to the NDIA – “specialised driving training” is a quote required item, which needs to be approved by NDIA and added as a line item to your NDIA plan under Capacity Building: improved daily living (Specialised driver training 15_046_0129_1_3).
Once you have written approval from the NDIA, you are able to book your lessons directly with the driving instructor. (Note – as at February 2022, this is taking months to gain approval).
4) On-road re-assessment to review progress
For some clients, an OT on-road re-assessment will be completed part-way through their lessons, to check that everything is progressing as it should be, and gain the evidence to confirm that the modifications will enable the person to be a safe driver in the long term.
5) OT Driver Assessor to submit vehicle mods application
A vehicle modifications application is then completed and submitted to the insurer. This will typically include a suite of documents including:
- copy of driver’s licence
- copy of QLD Transport Medical Certificate
- the vehicle modifications application and signed consent forms
- OT driving assessment report/s
- letter from the client indicating that they consent to their vehicle being modified
- copy of vehicle registration and insurance
- vehicle Safety Certificate / Roadworthy may be required (at client’s expense)
NB: insurers have varying criteria about age and kilometres of the vehicle, which is considered to be “suitable” to modify. NDIS require no older than 5 years and no more than 80,000km – however, when minor modifications are being completed (including hand controls) which can be transferred to the next vehicle, they will usually accept this as long as the Safety Certificate is also provided.
6) Wait!
Await approval of the vehicle modifications. (again, there may be lengthy wait times for NDIS Participants).
7) Installation, lessons, license/medical certificate review
- Following approval, modifications are installed into the vehicle.
- Driving lessons should be occurring at this time.
- License/medical certificate will also be reviewed – the OT driver assessor will liaise with the driving instructor, and determine when it will be appropriate to provide an updated report to the GP to recommend an upgrade to the medical certificate – to remove the restriction of “driving with driving instructor only”. So it is off to the GP again to upgrade the medical certificate and this has to be taken to QLD Transport for processing, and provide copies to the OT Driver Assessor and insurer.
8) Handover assessment
- When the vehicle modifications are completed, our process at Driving Well Occupational Therapy is to complete a handover assessment at the modifier, with the client, OT Driver Assessor and Driving Instructor, to take the modified car for a test drive, and ensure everything is set up and working as it should be for the client.
- The OT will review the compliance documents of the modifications.
- Some clients will be able to drive their vehicle home, however sometimes this is not possible if the client is not yet competent or if there are tweaks needed to the mods.
Note: in QLD, a Transport driving test is not required, however this is a requirement in other states. In QLD, we need to be confident that the client is driving at the QLD Transport driving test standard, and that if they did have to complete a test, that they are at passing level.
9) Further lessons as needed
Some clients will have another few lessons in their own modified vehicle to gain experience and confidence.
10) Sign-off
OT driver assessor will complete final on-road report and post-modification evaluation report – these will be sent to QLD Transport and the insurer.
A celebration is definitely in order after all this! And for Driving Well, the handover days are the absolute highlight for us, our “WHY FACTOR” – this is why we do what we do!
Vehicle modifications network - who is who in the Driving Well zoo
Suppliers:
- Total Ability https://totalability.com.au/products/hand-controls/
- Problem Management Engineering https://www.pmeautoconversions.com.au/driving-controls/hand-controls
- Mobility Engineering https://www.mobilityengineering.com.au/
Brisbane vehicle modifiers:
- Alternate Mobility https://www.alternatemobility.com.au/
- Driving Mobility (formerly Auto Extras) https://drivingmobility.com.au/
- KCF Disability Engineering http://www.kcfdisabilityengineering.com.au/
Specialised driving instructors in Greater Brisbane region:
- Ivor Booker, Driver Education and Training Services (south side and Ipswich): mechanical hand controls, and operates specialised vehicles from Alternate Mobility in partnership with Total Ability
- Lorraine Anthony: mechanical hand controls
- Darren Innes, 21st Century Driving School (north side): electronic hand controls
- Easy Start Driving School (Andrew Mitsi): electronic hand controls
- My Driving School – Moreton Bay region (Liz Beggs): electronic hand controls, including the Carospeed system.
Check out our website www.drivingwell.com.au and get in touch if you need support with driving and/or vehicle access with a medical condition or disability.
#drivingassessment #handcontrols #vehiclemodifications #transport #independence #safety #driving #NDIS #occupationaltherapy #brisbane
There is a wide range of vehicle modifications on the market which enable people with injury or disability to drive a vehicle and/or to access a vehicle.
Driver modifications:
- spinner knobs and other steering aids
- electronic steering aids eg steering knobs and satellite accelerators
- push/pull and push/pat hand controls
- over/under-ring accelerator
- indicator extension levers
- left foot accelerator
- automatic transmission conversion
Passenger / vehicle access modifications:
- wheelchair accessible conversions and fitouts
- wheelchair hoists and ramps
- lowered floors
- wheelchair tie-downs and docking stations/pins
- seating conversions
- wheelchair and scooter storage
So What do I do?
The general process with any vehicle modification is as follows:
1) Have an OT assessment and prescription from a qualified Occupational Therapist (must be a driving trained OT to prescribe driver mods). Prescription will usually require the team of client, OT, driving instructor and vehicle modifier to work together to determine the best option.
Clients returning to driving
2) Have lessons with the rehabilitation driving instructor to develop competence with the modifications
3) Have an OT on-road re-assessment if necessary
4) OT liaises with the driving instructor and informs GP/specialist that you have passed
5) Return to GP/specialist to gain new medical certificate,
6) Take updated medical certificate to QLD Transport to have licence endorsed with conditions “M” for medical condition and “V” for vehicle modification
All clients
7) Modifications must be installed and authorised by an approved officer
8) Modifications must also be reported to QLD Transport and a modification plate installed
Earlier in the year, Car Free Me was featured on Channel 9 News. This blog is shared from Car Free Me’s website – for information click here.
The reporters talked to the team about how to prepare for a car free life. Driving cessation is a big step for most people. But it doesn’t mean that it takes away your freedom and independence. In this two minute segment, Channel 9 introduces the Car Free Me program and how it can help senior drivers in Australia.
Watch the video: Older drivers in Queensland preparing for a car-free
What is Car Free Me?
Car Free Me is for people who are still driving and are considering stopping, and for those who have already stopped driving. It is an interactive and supportive program that runs for 6 weeks. Every week, a group of people gets together with their Car Free Me accredited coach. During each workshop we will give you with the building blocks to becoming car free.
“The important thing is that people take that time to plan for it, to think about stopping driving”, said Dr Theresa Scott, academic at The University of Queensland and member of the Car Free Me research team.
“We are here to support you in your decision and preparation for a car free life. We help you evaluate the options that suit your lifestyle so you can continue to do what you love, without needing a car.”
The participants so far have been very pleased with the program. A Brisbane workshop participant wrote: “I have learned about finding alternative means of transport, planning with more wisdom, the search for best retirement options. The information supplied, support and encouragement, professionalism of the program have all been very useful”.
Recommended reading: How does Car Free Me work?
When do I know I need to stop driving?
Did you know that elderly drivers are the safest drivers? Age is not a factor determining whether or not one should stop driving. However when you start facing new health challenges (like mobility issues and vision impairment), this is when you need to start thinking about alternatives.
At 79, Ross McKinnon still drives everyday and has a clean bill of health. But he told Channel 9 that “it’s important to recognise that everybody will have to make that change.” Safe mobility is essential to healthy ageing.
“Don’t leave it to the last minute to start preparing for your car free life.”
Car Free Me in regional areas of Australia
Everyone should be able to have access to the help they need. Thanks to telehealth trials, the Car Free Me program will be trialled outside of urban, metropolitan areas.
What is telehealth? The Department of Health defines it as “the use of telecommunication technology for the purpose of providing health education over a distance”. That is, you will be able to chat and see your Car Free Me coach using video-conferencing. Easy and effective.
Can I help you?
Please contact me at Driving Well Occupational Therapy if you have concerns about an elderly client’s / patient’s / loved one’s driving.
#olderdrivers #occupationaltherapy #practicaldrivingassessment #drivingcessation
My beautiful Great-Aunty Joanie (pictured here a few years ago with my son Henry, now 3) has travelled the world, loves going to the ballet and theatre, and has never driven. She has survived almost a century on planes, trains and bus tours, and more recently gets around with transport help from friends and family, and of course taxis.
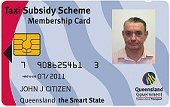
Recently, at 97 years young, she told me that she asked her doctor to assist her with obtaining the Taxi Subsidy Scheme to help her with transport costs, and was told she wasn’t eligible. So, I decided to have a closer look.
The TSS looks like an ID card and has your photo – you present this to the driver and at the end of the journey you are charged half the fare, up to a maximum of $25.
The eligibility criteria are fairly straight forward – except for Category 2 – Mobility Impairment.
It says that the person “has a physical disability or a medical condition that restricts the person from walking, unassisted and without a rest, 50m or less” or “has a physical disability or other medical condition requiring the person to carry treatment equipment which restricts them from walking unassisted and without a rest 50m, or requires someone else to carry the equipment”.
Confused yet? What does this mean?
In basic terms, the person applying for the taxi subsidy needs to have a medical condition that impacts on their mobility in one of the following ways:
- they need to use a mobility aid such as a walking stick or four wheeled walker
- they use the mobility aid for outdoor activities such as going to the doctor or going shopping
- they can’t walk more than 50m without an aid or a rest: this may be due to factors such as pain or shortness of breath
- they can’t go up and down 3 steps independently: typically can’t get on a bus or access train stations on their own
- they have had falls in the last 12 months
- they are at high risk of falls: to determine falls risk, a physiotherapist or occupational therapist can complete a Timed Up and Go (TUG) test – a TUG score of 12 seconds or more indicates that the person is at high risk of falls, and would be eligible for the taxi subsidy
- they carry treatment equipment such as an oxygen cylinder
- they are assessed by a physiotherapist or occupational therapist as requiring “1 x assist mobility”: meaning that they need another person to physically assist them to mobilise
What else do you need?
A GP, occupational therapist or physiotherapist can complete the TSS application for people eligible for Categories 1 and 2 (severe mobility impairment). The form and details to submit the TSS application are on the website. You also need two passport-sized photographs, witnessed by a health professional / JP / lawyer / police officer / pharmacist.
“It’s the best thing!”
Aunty Joanie
You’d think at 97 years of age it would be a no-brainer to be given access to the taxi subsidy!
I was able to demonstrate Aunty Joanie’s eligibility on Category 2: Mobility Impairment with the following information:
- Aunty Joanie’s health has actually been pretty good and she doesn’t have any medical conditions causing shortness of breath or pain
- at the point of application she hadn’t had any recent falls, but was a bit unsteady on her feet
- she uses a four-wheeled walker when shopping alone
- she was no longer safely able to access steps on her own
- I performed a TUG and her score was 18 seconds, indicating she was at high risk of falls
3 weeks
Aunty Joanie received her Taxi Subsidy Scheme card within 3 weeks of my visit to complete her application. She happily waved it at me and said it was “the best thing” and has used it successfully to go to her local shopping centre and favourite cafe. Love her.
Can I help you?
Please contact me at Driving Well Occupational Therapy if you need a hand in obtaining the Taxi Subsidy Scheme.
"*" indicates required fields
- Resources
- Insights
- Forms
- Driver Focus App
Driving Well Occupational Therapy is a busy practice that provides OT driving assessment and vehicle modification services for people with medical conditions and injuries in Brisbane, Ipswich and northern Gold Coast. We service clients who are self-funding, NDIS and other compensable (WorkCover, NIISQ, TAC, iCare).
On behalf of the team at Driving Well Occupational Therapy and in the spirit of reconciliation, I acknowledge the Traditional Custodians of Turrbul and Yuggera country, where our team live and serve the majority of our clients, as well as to all Traditional Custodians of country throughout Australia and their connections to the land, sea and community. I pay my respects to Elders past and present, and extend that respect to all First Nations people today.
On behalf of the team at Driving Well Occupational Therapy and in the spirit of reconciliation, I acknowledge the Traditional Custodians of Turrbul and Yuggera country, where our team live and serve the majority of our clients, as well as to all Traditional Custodians of country throughout Australia and their connections to the land, sea and community. I pay my respects to Elders past and present, and extend that respect to all First Nations people today.